Unfortunately, periodontal disease is very common in adults. The symptoms of periodontal disease are bleeding, red or swollen gums and can also include bad odor, discomfort on chewing, and loose or shifting teeth. There are many factors that contribute to this chronic infection, such as poor oral hygiene, stress, smoking, medical conditions like diabetes, or inherited genetic tendencies. Since the silent symptoms of periodontal disease often only become noticeable in the more moderate-to-advanced stages, it is essential to have regular check-ups and professional cleaning to preserve your oral health and help keep your natural teeth for a lifetime.
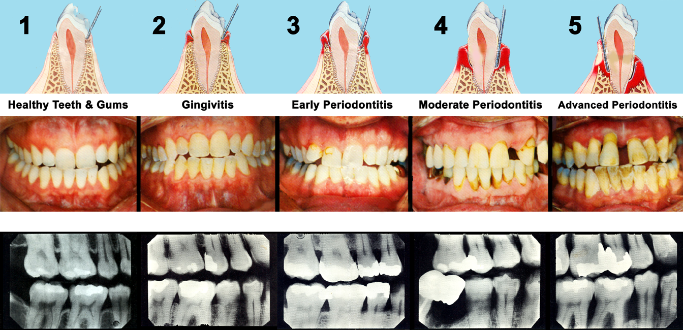
The word periodontal literally means "around the tooth." Periodontal disease is a chronic bacterial infection that attacks the gums and bone supporting the teeth. It begins when the bacteria in plaque (the sticky, colorless film that constantly forms on your teeth) causes the gums to become inflamed. If plaque is not removed, it turns into calculus (tartar). When plaque and calculus are not removed, they begin to destroy the gums and bone. Periodontal disease is characterized by red, swollen, and bleeding gums. In the mildest form of the disease, gingivitis, the gums redden, swell and bleed easily. There is usually little or no discomfort. Gingivitis is often caused by inadequate oral hygiene. Gingivitis is reversible with professional treatment and good oral home care.
Untreated gingivitis can advance to periodontitis. With time, plaque can spread and grow below the gum line. Toxins produced by the bacteria in plaque irritate the gums. The toxins stimulate a chronic inflammatory response in which the body in essence turns on itself, and the tissues and bone that support the teeth are broken down and destroyed. Gums separate from the teeth, forming pockets (spaces between the teeth and gums) that become infected. As the disease progresses, the pockets deepen and more gum tissue and bone are destroyed. Often, this destructive process has very mild symptoms. Eventually, teeth can become loose and may have to be removed.
Not only is periodontitis the number one reason for tooth loss, research suggests that there may be a link between periodontal disease and other diseases such as, stroke, bacterial pneumonia, diabetes, cardiovascular disease, and increased risk during pregnancy. Researchers are determining if inflammation and bacteria associated with periodontal disease affects these systemic diseases and conditions. Smoking also increases the risk of periodontal disease.
Signs and symptoms of periodontal disease:
- Bleeding gums – Gums should never bleed, even when you brush vigorously or use dental floss.
- Loose teeth – Also caused by bone loss or weakened periodontal fibers (fibers that support the tooth to the bone).
- New spacing between teeth – Caused by bone loss.
- Persistent bad breath – Caused by bacteria in the mouth.
- Pus around the teeth and gums – Sign that there is an infection present.
- Receding gums – Loss of gum around a tooth.
- Red and puffy gums – Gums should never be red or swollen.
- Tenderness or Discomfort – Plaque, calculus, and bacteria irritate the gums and teeth.
- Changes in the fit of partial dentures - Caused by bone loss.
Risk factors for periodontal disease:
- Smoking/Tobacco use
- Stress
- Genetics
- Pregnancy/Puberty
- Medications
- Clenching or Grinding your teeth
- Diabetes
- Poor Nutrition
- Other Systemic Diseases
Periodontal Disease and Overall Health
The link between you oral health and your overall health: A recent Surgeons General’s Report and a growing number of research studies suggest that there are links between chronic oral infections(periodontitis) and diabetes, heart and lung disease, stroke and even low-birth- weight babies. Taking good care of you oral health today may protect your overall health in days to come.
Cardiovascular Diseases
Oral bacteria can affect the heart when they enter the bloodstream, attaching to fatty plaques in the coronary arteries (heart blood vessels) and contributing to clot formation. Researchers have found that people with periodontal disease are almost twice as likely to suffer from coronary artery disease as those without periodontal disease.
Diabetes
For years we’ve known that people with diabetes are more likely to have periodontal disease than people without diabetes. Recently, research has emerged suggesting that the relationship goes both ways – periodontal disease may make it more difficult for people who have diabetes to control their blood sugar. Severe periodontal disease can increase blood sugar, putting diabetics at increased risk for complications. If you are among the 16 million Americans who live with diabetes or are at risk for diabetes or periodontal disease, see a periodontist for an evaluation.
Pregnancy
Pregnant women who have periodontal disease may be seven times more likely to have a baby that is born too early and too small. Periodontal disease is an infection and all infections are cause for concern during pregnancy because they pose a risk to the health of the baby. If you are thinking about becoming pregnant, be sure to include an evaluation with a periodontist as part of your prenatal care.
Osteoporosis
Researchers have suggested a link between osteoporosis and bone loss in the jaw. Studies suggest that osteoporosis may lead to tooth loss because the density of the bone that supports the teeth may be decreased, which means the teeth no longer have a solid foundation. However, hormone replacement therapy may offer some protection.
Patients on bisphosphonate therapy may be at increased risk for a condition known as osteonecrosis of the jaw. This condition can be worsened by invasive dental procedures. If you are taking bisphosphonates and are going to be receiving periodontal surgery or other procedures, talk to your periodontist first.
Scientists have found that bacteria that grow in the oral cavity can be aspirated into the lung to cause respiratory diseases such as pneumonia, especially in people with periodontal disease. This discovery leads researchers to believe that these bacteria can travel from the oral cavity into the lungs to cause infection.
Q. How can I tell if I have gingivitis or periodontitis (gum diesease)?
Four out of five people have periodontal disease and don’t know it! Most people are not aware of it because the disease is usually painless in the early stages. Unlike tooth decay, which often causes discomfort, it is possible to have periodontal disease without noticeable symptoms. Having regular dental check-ups and periodontal examinations are very important and will help detect if periodontal problems exist.
Periodontal disease begins when plaque, a sticky, colorless, film of bacteria, food debris, and saliva, is left on the teeth and gums. The bacteria produce toxins (acids) that inflame the gums and slowly destroy the bone. Brushing and flossing regularly and properly will ensure that plaque is not left behind to do its damage.
Other than poor oral hygiene, there are several other factors that may increase the risk of developing periodontal disease:
- Smoking or chewing tobacco – Tobacco users are more likely than nonusers to form plaque and tartar on their teeth.
- Certain tooth or appliance conditions – Bridges that no longer fit properly, crowded teeth, or defective fillings that may trap plaque and bacteria.
- Many medications – Steroids, cancer therapy drugs, blood pressure meds, oral contraceptives. Some medications have side affects that reduce saliva, making the mouth dry and plaque easier to adhere to the teeth and gums.
- Pregnancy, oral contraceptives, and puberty – Can cause changes in hormone levels, causing gum tissue to become more sensitive to bacteria toxins.
- Systemic diseases – Diabetes, blood cell disorders, HIV / AIDS, etc.
- Genetics may play role – Some patients may be predisposed to a more aggressive type of periodontitis. Patients with a family history of tooth loss should pay particular attention to their gums.
Signs and Symptoms of Periodontal Disease
- Red and puffy gums - Gums should never be red or swollen.
- Bleeding gums - Gums should never bleed, even when you brush vigorously or use dental floss.
- Persistent bad breath - Caused by bacteria in the mouth.
- New spacing between teeth - Caused by bone loss.
- Loose teeth - Also caused by bone loss or weakened periodontal fibers (fibers that support the tooth to the bone).
- Pus around the teeth and gums - Sign that there is an infection present.
- Receding gums - Loss of gum around a tooth.
- Tenderness or Discomfort - Plaque, calculus, and bacteria irritate the gums and teeth.
Good oral hygiene, a balanced diet, and regular dental visits can help reduce your risk of developing periodontal disease.
FAQ:
Q. What are pockets?
Bleeding gums are one of the signs of gum disease. Think of gum tissue as the skin on your hand. If your hands bled every time you washed them, you would know something was wrong.
Q: I'm over 55. Does this mean I'm more likely to get periodontal disease?
Your chances of developing periodontal disease increase considerably as you get older. More than half of people aged 55 and older have periodontitis. The good news is that research suggests that these higher rates may be related to risk factors other than age. So, periodontal disease is not an inevitable part of aging. Risk factors that may make older people more susceptible include general health status, diminished immune status, medications, depression, worsening memory, diminished salivary flow, functional impairments and change in financial status.
eriodontist?
Q: How often should I brush and floss?
Brushing and flossing help control the plaque and bacteria that cause dental disease.
Plaque is a film of food debris, bacteria, and saliva that sticks to the teeth and gums. The bacteria in plaque convert certain food particles into acids that cause tooth decay. Also, if plaque is not removed, it turns into calculus (tartar). If plaque and calculus are not removed, they begin to destroy the gums and bone, causing periodontal (gum) disease.
Plaque formation and growth is continuous and can only be controlled by regular brushing, flossing, and the use of other dental aids.
Tooth brushing – Brush your teeth at least twice a day (especially before going to bed at night) with an ADA approved soft bristle brush and toothpaste.
- Brush at a 45 degree angle to the gums, gently using a small, circular motion, ensuring that you always feel the bristles on the gums.
- Brush the outer, inner, and biting surfaces of each tooth.
- Use the tip of the brush head to clean the inside front teeth.
- Brush your tongue to remove bacteria and freshen your breath.
Electric toothbrushes are also recommended. They are easy to use and can remove plaque efficiently. Simply place the bristles of the electric brush on your gums and teeth and allow the brush to do its job, several teeth at a time.
Flossing - Daily flossing is the best way to clean between the teeth and under the gumline. Flossing not only helps clean these spaces, it disrupts plaque colonies from building up, preventing damage to the gums, teeth, and bone.
- Take 12-16 inches (30-40cm) of dental floss and wrap it around your middle fingers, leaving about 2 inches (5cm) of floss between the hands.
- Using your thumbs and forefingers to guide the floss, gently insert the floss between teeth using a sawing motion.
- Curve the floss into a “C” shape around each tooth and under the gumline. Gently move the floss up and down, cleaning the side of each tooth.
Floss holders are recommended if you have difficulty using conventional floss.
Rinsing - It is important to rinse your mouth with water after brushing, and also after meals if you are unable to brush. If you are using an over-the-counter product for rinsing, it’s a good idea to consult with your dentist or dental hygienist on its appropriateness for you
Q: Why is it important to use dental floss?
Brushing our teeth removes food particles, plaque, and bacteria from all tooth surfaces, except in between the teeth. Unfortunately, our toothbrush can’t reach these areas that are highly susceptible to decay and periodontal (gum) disease.
Daily flossing is the best way to clean between the teeth and under the gumline. Flossing not only helps clean these spaces, it disrupts plaque colonies from building up, preventing damage to the gums, teeth, and bone.
Plaque is a sticky, almost invisible film that forms on the teeth. It is a growing colony of living bacteria, food debris, and saliva. The bacteria produce toxins (acids) that cause cavities and irritate and inflame the gums. Also, when plaque is not removed above and below the gumline, it hardens and turns into calculus (tartar). This will further irritate and inflame the gums and also slowly destroy the bone. This is the beginning of periodontal disease.
How to floss properly:
- Take 12-16 inches (30-40cm) of dental floss and wrap it around your middle fingers, leaving about 2 inches (5cm) of floss between the hands.
- Using your thumbs and forefingers to guide the floss, gently insert the floss between teeth using a sawing motion.
- Curve the floss into a “C” shape around each tooth and under the gumline. Gently move the floss up and down, cleaning the side of each tooth.
Floss holders are recommended if you have difficulty using conventional floss.
Daily flossing will help you keep a healthy, beautiful smile for life!
Q: What should I do if I have bad breath?
Bad breath (halitosis) can be an unpleasant and embarrassing condition. Many of us may not realize that we have bad breath, but everyone has it from time to time, especially in the morning.
There are various reasons one may have bad breath, but in healthy people, the major reason is due to microbial deposits on the tongue, especially the back of the tongue. Some studies have shown that simply brushing the tongue reduced bad breath by as much as 70 percent.
Q: What may cause bad breath?
- Morning Time - Saliva flow almost stops during sleep and its reduced cleansing action allows bacteria to grow, causing bad breath.
- Certain Foods - Garlic, onions, etc. Foods containing odor-causing compounds enter the blood stream; they are transferred to the lungs, where they are exhaled.
- Poor Oral Hygiene Habits - Food particles remaining in the mouth promote bacterial growth.
- Periodontal (gum) disease - Colonies of bacteria and food debris residing under inflamed gums.
- Dental Cavities and improperly fitted dental appliances - May also contribute to bad breath.
- Dry Mouth (Xerostomia) - May be caused by certain medications, salivary gland problems, or continuous mouth breathing.
- Tabacco products - Dry the mouth, causing bad breath.
- Dieting - Certain chemicals called ketones are released in the breath as the body burns fat.
- Dehydration, hunger, and missed meals - Drinking water and chewing food increases saliva flow and washes bacteria away.
- Certain medical conditions and illnesses - Diabetes, liver and kidney problems, chronic sinus infections, bronchitis, and pneumonia are several conditions that may contribute to bad breath.
Keeping a record of what you eat may help identify the cause of bad breath. Also, review your current medications, recent surgeries, or illnesses with you dentist.
Q: What can I do to prevent bad breath?
- Practice good oral hygiene - Brush at least twice a day with an ADA approved fluoride toothpaste and toothbrush. Floss daily to remove food debris and plaque from in between the teeth and under the gumline. Brush or use a tongue scraper to clean the tongue and reach the back areas. Replace your toothbrush every 2 to 3 months. If you wear dentures or removable bridges, clean them thoroughly and place them back in your mouth in the morning.
- See your dentist regularly - Get a check-up and cleaning at least twice a year. If you have or have had periodontal disease, your dentist will recommend more frequent visits.
- Stop smoking/chewing tobacco - Ask your dentist what they recommend to help break the habit.
- Drink water frequently - Water will help keep your mouth moist and wash away bacteria.
- Use mouthwash/rinses - Some over-the-counter products only provide a temporary solution to mask unpleasant mouth odor. Ask your dentist about antiseptic rinses that not only alleviate bad breath, but also kill the germs that cause the problem.
In most cases, your dentist can treat the cause of bad breath. If it is determined that your mouth is healthy, but bad breath is persistent, your dentist may refer you to your physician to determine the cause of the odor and an appropriate treatment plan.
Q : Is there a relationship between tobacco use and periodontal disease?
Studies have shown that tobacco use may be one of the most significant risk factors in the development and progression of periodontal disease. Smokers are much more likely than non-smokers to have calculus form on their teeth, have deeper pockets between the teeth and gums and lose more of the bone and tissue that support the teeth. In addition, smokers tend to heal less favorably than nonsmokers.
Q: What does heart disease and other medical conditions have to do with periodontal (gum) disease?
Many people are unaware that having periodontal disease (the destruction of gum tissue and bone that hold our teeth in place) can affect your overall health. Periodontal disease is one of the most common infections; often more prevalent than the common cold! Periodontal disease is not only the number one reason people lose teeth; it can also affect the health of your body!
There are numerous studies that have looked into the correlation between gum disease and major medical conditions. These studies suggest people with periodontal disease are at a greater risk of systemic disease and indicate that periodontal disease may cause oral bacteria to enter the bloodstream and travel to major organs and begin new infections. Research suggests that periodontal bacteria in the blood stream may:
- Contribute to the development of heart disease
- Increase the risk of stroke
- Compromise the health of those that have diabetes or respiratory diseases
- Increase a woman’s risk of having a preterm, low-birth weight baby
Researchers conclude there is still much research to be done to understand the link between periodontal disease and systemic diseases, but enough research has been done to support that infections in the mouth can play havoc elsewhere in the body.
To ensure a healthy, disease-free mouth, we recommend the importance of regular dental check-ups and cleanings, which include a periodontal evaluation. Also, diligent home care and a proper diet can help reduce the plaque and bacteria in the mouth.
Remember….the mouth body connection! Taking care of your oral health may contribute to your overall medical health!
Q: What are my options if I have missing teeth?
With many state-of-the-art dental treatments and prevention options available in dentistry today, there are fewer reasons for having to extract (remove) teeth. When something does go wrong with a tooth, Dr will try to do everything possible to restore the tooth to its original function. Removing a tooth is the last option because we know that removal may lead to severe and costly dental and cosmetic problems if the tooth is not replaced.
Losing a tooth can be a very traumatic experience and it’s very unfortunate when it does happen. Injury, accident, fracture, severe dental decay, and gum disease are the major reasons for having to remove a tooth. If teeth are lost due to injury or have to be removed, it is imperative that they be replaced to avoid cosmetic and dental problems in the future.
When a tooth is lost, the jaw bone that helped to support that tooth begins to atrophy, causing the teeth on either side to shift or tip into the open space of the lost tooth. Also, the tooth above or below the open space will start to move towards the open space because there is no opposing tooth to bite on. These movements may create problems such as decay, gum disease, excessive wear on certain teeth, and TMJ (jaw joint) problems. These problems and movements do not result immediately, but will eventually appear, compromising your chewing abilities, the health of your bite, and the beauty of your smile.
Options for replacement of missing teeth:
Removable bridges - This type of bridge replaces one or more missing teeth. They are usually made of tooth-colored, artificial teeth combined with metal clasps that hook onto adjacent natural teeth. Removable bridges are the most economical option for replacing missing teeth, but may be the least aesthetically pleasing. This is because the metal clasps on the appliances are often impossible to completely conceal. In addition, fit and function may be compromised.
Fixed bridges - This type of bridge is generally made of porcelain or composite material and is anchored (cemented) permanently to a natural teeth adjacent to the missing tooth site. The benefit of this type of bridge is that it is fixed (not removable) and it is very sturdy. The disadvantage is that in order to create a fixed appliance, two healthy, natural teeth will have to be grounded down and crowned (capped) to hold the bridge in place.
Dentures - This type of tooth replacement is used when most or all of the natural teeth are missing in one dental arch. Dentures are removable artificial teeth that are made to closely resemble the patients’ original teeth.
Implants - Are a great way to replace one or more missing teeth. They may also be great to support ill fitting dentures. A dental implant is an artificial root that is surgically placed into the jaw bone to replace a missing tooth. An artificial tooth is placed on the implant, giving the appearance and feel of a natural tooth. Implants are very stable, durable, and are the most aesthetically pleasing tooth replacement option.